Günlü, Serhat
Loading...

Profile URL
Name Variants
Job Title
Dr. Öğr. Üyesi
Email Address
Main Affiliation
Department of Internal Medical Sciences / Dahili Tıp Bilimleri Bölümü
Status
Current Staff
Website
ORCID ID
Scopus Author ID
Turkish CoHE Profile ID
Google Scholar ID
WoS Researcher ID
Sustainable Development Goals
17
PARTNERSHIPS FOR THE GOALS

0
Research Products
2
ZERO HUNGER

0
Research Products
5
GENDER EQUALITY

0
Research Products
6
CLEAN WATER AND SANITATION

0
Research Products
13
CLIMATE ACTION

0
Research Products
10
REDUCED INEQUALITIES

0
Research Products
16
PEACE, JUSTICE AND STRONG INSTITUTIONS

0
Research Products
8
DECENT WORK AND ECONOMIC GROWTH

0
Research Products
15
LIFE ON LAND

0
Research Products
3
GOOD HEALTH AND WELL-BEING

7
Research Products
9
INDUSTRY, INNOVATION AND INFRASTRUCTURE

0
Research Products
14
LIFE BELOW WATER

1
Research Products
4
QUALITY EDUCATION

0
Research Products
1
NO POVERTY

0
Research Products
7
AFFORDABLE AND CLEAN ENERGY

0
Research Products
11
SUSTAINABLE CITIES AND COMMUNITIES

0
Research Products
12
RESPONSIBLE CONSUMPTION AND PRODUCTION

0
Research Products

This researcher does not have a Scopus ID.

This researcher does not have a WoS ID.

Scholarly Output
25
Articles
22
Views / Downloads
127/2934
Supervised MSc Theses
0
Supervised PhD Theses
0
WoS Citation Count
19
Scopus Citation Count
23
WoS h-index
3
Scopus h-index
3
Patents
0
Projects
0
WoS Citations per Publication
0.76
Scopus Citations per Publication
0.92
Open Access Source
16
Supervised Theses
0
Google Analytics Visitor Traffic
| Journal | Count |
|---|---|
| Journal of Electrocardiology | 2 |
| Aging Clinical and Experimental Research | 2 |
| Artuklu International Journal of Health Sciences | 2 |
| International Journal of Cardiovascular Sciences | 2 |
| Black Sea Journal of Health Science | 1 |
Current Page: 1 / 5
Scopus Quartile Distribution
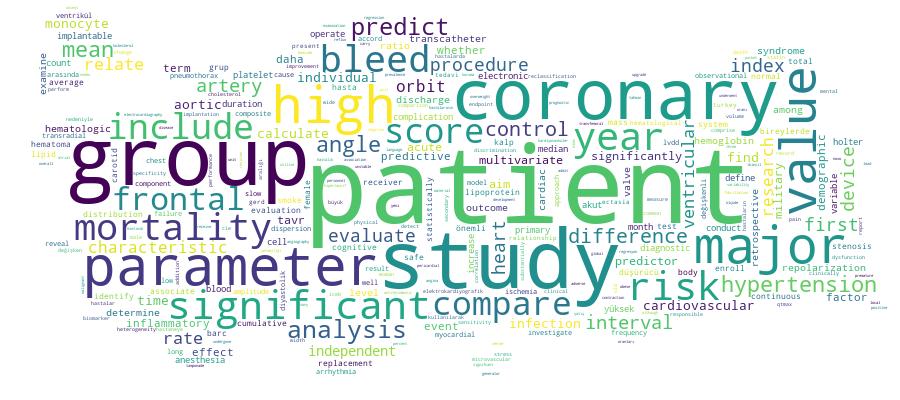
Competency Cloud
25 results
Scholarly Output Search Results
Now showing 1 - 10 of 25
Article Citation - WoS: 2Citation - Scopus: 2Evaluation of Hematological Parameters After Transcatheter Aortic Valve Replacement(Sage Journals, 2023) Karahan, Mehmet Zülkif; Aktan, Adem; Güzel, Tuncay; Kılıç, Raif; Günlü, Serhat; Demir, Muhammed; Ertaş, FarukAlthough transcatheter aortic valve replacement (TAVR) is safe and effective, mortality and bleeding events post procedure are important. The present study investigated the changes in hematologic parameters to evaluate whether they predict mortality or major bleeding. We enrolled 248 consecutive patients (44.8% male; mean age 79.0 ± 6.4 years) undergoing TAVR. In addition to demographic and clinical examination, blood parameters were recorded before TAVR, at discharge, 1 month and 1 year. Hemoglobin levels before TAVR 12.1 ± 1.8 g/dL, 10.8 ± 1.7 g/dL at discharge, 11.7 ± 1.7 g/dL at first month, 11.8 ± 1.4 g/dL at first year (Hemoglobin values compared with pre-TAVR, P < .001, P = .019, P = .047, respectively). Mean platelet volume (MPV) before TAVR 8.72 ± 1.71 fL, 8.16 ± 1.46 fL at discharge, 8.09 ± 1.44 fL at first month, 7.94 ± 1.18 fL at first year (MPV values compared with pre-TAVR, P < .001, P < .001, P < .001, respectively). Other hematologic parameters were also evaluated. Hemoglobin, platelet count, MPV, and red cell distribution width before the procedure, at discharge, and at the first year did not predict mortality and major bleeding in receiver operating characteristic analysis. After multivariate Cox regression analysis, hematologic parameters were not independent predictors of in-hospital mortality, major bleeding, and death at 1 year after TAVR.Presentation Predicting the mortality in patients with carotid artery stenosis by monocyte to high density lipoprotein ratio(2023) Günlü, SerhatIntroduction: Background: Monocytes, which produce a variety of cytokines and molecules, interact with platelets and endothelial cells, causing inflammatory and thrombotic pathways to become worse. Macrophage migration and oxidation of low-density lipoprotein cholesterol molecules are both inhibited by high-density lipoprotein cholesterol (HDL-C). HDL-C neutralizes monocytes' pro-inflammatory and pro-oxidant effects through several mechanisms. As a result, characteristics like the monocyte to HDL-C ratio (MHR) may reveal a patient's inflammatory status. Objective: The development of carotid artery stenosis (CAS) is influenced by inflammation, oxidative stress, and endothelial dysfunction. Recent research suggests that inflammatory biomarkers are important for assessing mortality in carotid artery stenosis. This study aims to determine the association between MHR and mortality after carotid artery stenting. Tools and Method: We enrolled 260 patients with CAS who underwent carotid artery stenting between 2019 and 2021. MHR was calculated using the formula: the monocyte value dividing by the high-density lipoprotein cholesterol value. According to 30-day mortality, the patients were divided into two groups; surviving and non-surviving. Monocyte counts, HDL-C, and MHR values were compared between the groups. Results: The patient group had significantly higher monocyte counts and lower HDL levels than the control group, resulting in higher MHR values. In addition, non-surviving patients had a higher monocyte count and MHR value, as well as a lower HDL-C level (p<0.001). In patients with CAS, the MHR value was also found to be a significant independent determinant of 30-day mortality (p<0.001). MHR had the optimum cut-off value of 17.52 with 78.3% sensitivity and 83.4% specificity (AUC:0.724, p<0.001) for predicting 30-day mortality in patients with CAS. Comparison of the monocyte count, HDL level, and MHR value according to the mortality within the 30 days. Non-surviving group n=48 Surviving group n=212 P-values Monocyte (x109 µL) 915.42±53.21 524.03±9.98 <0.001 HDL-C (mg/dL) 37.03±1.16 46.22±0.9 <0.001 MHR 18.86±5.25 12.21±2.21 <0.001 Values are presented as mean ± SD and median [interquartile range]. HDL-C; high-density lipoprotein cholesterol, MHR; monocyte to high-density lipoprotein ratio. Discussion: Conclusion: In patients with CAS, a high MHR value was found to be an independent predictor of 30-day mortality.Article Citation - WoS: 3The prognostic value of ORBIT risk score in predicting major bleeding in patients with acute coronary syndrome(ELSEVIER, 2023) Günlü, Serhat; Arpa, Abdulkadir; Kayan, Fethullah; Güzel, Tuncay; Kılıç, Raif; Aktan, Adem; Bernas, Altıntaş; Karahan, Mehmet ZülkifBackground: The most significant adverse effect of antithrombotic medication in acute coronary syndrome (ACS) is major bleeding, which is related to increased mortality. Studies on ORBIT risk score in predicting major bleeding in ACS patients are limited. Objective: This research aimed to examine whether the ORBIT score calculated at the bedside can identify major bleeding risk in patients with ACS. Methods: This research was retrospective, observational, and conducted at a single center. Analyses of receiver operating characteristics (ROC) were utilized to define the diagnostic value of CRUSADE and ORBIT scores. The predictive performances of the two scores were compared using DeLong's method. Discrimination and reclassification performances were evaluated by the integrated discrimination improvement (IDI), and net reclassification improvement (NRI). Results: The study included 771 patients with ACS. The mean age was 68.7 ± 8.6 years, with 35.3 % females. 31 patients had major bleeding. Twenty-three of these patients were BARC 3 A, five were BARC 3 B, and three were BARC 3 C. Bleeding history [OR (95 % CI), 2.46 (1.02–5.94), p = 0.021], hemoglobin levels [OR (95 % CI), 0.54 (0.45–0.63), p < 0.001], and age > 74 years [OR (95 % CI), 1.03 (1.01–1.06), p = 0.039] were independent predictors of major bleeding. The ORBIT score was an independent predictor of major bleeding in the multivariate analysis: continuous variables [OR (95 % CI), 2.53 (2.61–3.95), p < 0.001] and risk categories [OR (95 % CI), 3.06 (1.69–5.52), p < 0.001]. Comparison of c-indexes for major bleeding events revealed a non-significant difference for the discriminative ability of the two tested scores (p = 0.07) with a continuous NRI of 6.6 % (p = 0.026) and an IDI of 4.2 % (p < 0.001). Conclusion: In ACS patients, the ORBIT score independently predicted major bleeding.Book Part Akut Kalp Yetmezliğinde Tedavi Yaklaşımı(AKADEMİSYEN, 2023) Günlü, SerhatGIRIŞ Akut Kalp Yetmezliği (AKY) hastanın acil tıb- bi yardım alması için yeterince şiddetli bir kli- nik duruma, plansız bir hastaneye yatışa veya acil servis başvurusuna yol açan kalp yetmezliği semptomlarının ve/veya belirtilerinin hızlı veya aşamalı olarak başlamasını ifade eder (1). AKY’li hastalarının tedavilerinin planlanması için acil değerlendirilmesi gerekir. AKY, 65 yaş üstü kişi- lerde hastaneye yatışların önde gelen nedenidir (2). Yüksek mortalite ve tekrarlayan hastaneye yatış oranları mevcuttur. Hastane içi ölüm oranı %4 ila %10 arasında değişmektedir (3). Tabur- culuk sonrası 1 yıllık ölüm oranı %25-30, ölüm veya tekrar yatış oranları %45’ten fazladır (4). AKY, yeni başlayan KY’nin ilk belirtisi olabilir veya daha sıklıkla kronik KY’nin akut dekom- pansasyonuna bağlı ortaya çıkabilir (5). Akut de- kompanse kronik KY’si olan hastalarla akut pul- moner ödemli hastalar karşılaştırıldığında, akut pulmoner ödemi olanlar daha yüksek hastane içi mortaliteye sahiptirler ancak taburculuk sonra- sı mortalite ve yeniden hastaneye yatış oranları daha düşüktür (6). AKY’nin en sık tetikleyici fak- törleri atriyal fibrilasyon, akut MI veya iskemi, ilaç alımının (diüretik) kesilmesi, artmış sodyum yükü,miyokard fonksiyon bozukluklarına sebep olan ilaçlar ve aşırı fiziki efordur (7). Önceden var olan kardiyak disfonksiyonu olan hastalarda spesifik dış faktörler (anemi, GİS kanama, enfeksiyon vb.) AKY’yi hızlandırabilir (8).Article Kardiyovasküler Hastalık Yüksek Riskine Sahip Bireylerde Lipit Düşürücü İlaçların Etkinliği(2024) Kayan, Fethullah; Günlü, SerhatAmaç: Lipid düşürücü tedavinin optimal yönetimi, ikincil koruma altındaki hastalarda kardiyovasküler (KV) riskin azaltılmasında kritik bir rol oynamaktadır. Yüksek doz statinler, ezetimib ve nispeten yeni PCSK9 inhibitörleri (PCSK9i), bu hastalarda LDL kolesterol (LDL-K) tedavi hedeflerine ulaşmada etkinlik göstermiştir. Ancak, etkinliklerini destekleyen önemli kanıtlara rağmen, bu müdahaleler özellikle düşük hasta uyum düzeyleri nedeniyle önemli ölçüde yeterince kullanılmamaktadır. Dahası, kolesterol düşürücü tedavinin genel etkinliği ve ikincil koruma hastalarının düzenli bir lipid profili elde etme oranı hakkında sınırlı veri bulunmaktadır. Bu nedenle bu çalışmanın temel amacı, bu hasta grubundaki lipid düşürücü tedavi durumunu değerlendirmekti. Yöntemler: Çalışma, kardiyovasküler hastalık ikincil koruma geçmişi olan hastalara odaklanarak, Nisan 2021 ile Mart 2023 tarihleri arasında Mardin Artuklu Üniversitesi, Mardin Eğitim ve Araştırma Hastanesi’nde yapıldı. Çalışmada, reçetelenen kolesterol düşürücü ilaçlar, statin kullanımının yetersizliğine katkıda bulunan faktörler ve lipid profilinin açıklanması incelendi. Bulgular: 872 hasta çalışmaya dahil edildi. Hastaların %86,8'i statin (statin ile birlikte %5,2'si ezetimib ve %3,4'ü fibrat) kullanırken, %13,2'si herhangi bir lipid düşürücü tedavi almadı. Statin kullananların %64'ü yüksek dozda ilaç alıyordu. LDL-K değerleri 452 hastada değerlendirildi ve sadece %30'u önerilen 70 mg/dL altında bulunmaktaydı. Sonuç: İkincil korunma hastalarının yer aldığı bu araştırmada, katılımcıların yarısından biraz fazlası yüksek doz statin alırken, ihmal edilebilir bir oran ezetimib tedavisi almıştır. Endişe verici bir şekilde, hastaların üçte ikisinden fazlası, LDL-K değerleri terapötik aralıktan önemli ölçüde sapma gösterdi ve bu durum, lipid profilleri ile klinik kılavuzlar tarafından önerilen değerler arasında önemli bir boşluk olduğunu göstermektedir.Article Citation - Scopus: 1The predictive effect of shock index on mortality in patients with acute heart failure(AME Publishing, 2023) Günlü, Serhat; Kayan, Fethullah; Karahan, Mehmet ZülkifBackground: The predictive usefulness of the shock index (SI), which is determined as a proportion of heart rate (HR) to systolic blood pressure (SBP), and age-adjusted SI (SI × age) for clinical outcomes other than mortality in acute heart failure (AHF) is not well established. This research aimed to examine whether SI and SI × age measured non-invasively at a patient’s bedside can identify mortality risk in patients admitted to the coronary care unit (CCU) with AHF. Methods: This research was carried out as a retrospective case-control study. Indices were calculated. The receiving operating characteristic (ROC) and Youden index were applied to calculate the optimal SI and SI × age cut-off for estimating mortality. Using multivariate analysis to determine independent indicators of mortality in patients with AHF. Results: A total of 1,468 patients who were hospitalized at the CCU with AHF were included. The population’s median age was 81 (73–91) years and 53.7% were male. In the survivor group, the median SI was 0.6 (0.5–0.75), and the median SI × age was 46 (38–58). In the non-survivor group, the median SI was 0.62 (0.55–0.81) and the median SI × age was 53 (44–66). According to the Youden index, the best value of SI was 0.56 with a specificity of 46% and a sensitivity of 70%, and the best value of SI × age was 44.8 with a specificity of 48% and a sensitivity of 76%. In the multivariate analysis, the power of SI × age to predict mortality was 2.39 times greater than other independent predictors. Conclusions: SI and SI × age calculated in the CCU may be valuable prognostic markers for identifying AHF patients at high risk for adverse outcomes.Article Citation - WoS: 3Citation - Scopus: 3The prognostic value of ORBIT risk score in predicting major bleeding in patients with acute coronary syndrome(ScienceDirect, 2023) Günlü, Serhat; Arpa, Abdulkadir; Kayan, Fethullah; Güzel, Tuncay; Kılıç, Raif; Aktan, Adem; Altintaş, Bernas; Karahan, Mehmet ZülkifBackground: The most significant adverse effect of antithrombotic medication in acute coronary syndrome (ACS) is major bleeding, which is related to increased mortality. Studies on ORBIT risk score in predicting major bleeding in ACS patients are limited. Objective: This research aimed to examine whether the ORBIT score calculated at the bedside can identify major bleeding risk in patients with ACS. Methods: This research was retrospective, observational, and conducted at a single center. Analyses of receiver operating characteristics (ROC) were utilized to define the diagnostic value of CRUSADE and ORBIT scores. The predictive performances of the two scores were compared using DeLong's method. Discrimination and reclassification performances were evaluated by the integrated discrimination improvement (IDI), and net reclassification improvement (NRI). Results: The study included 771 patients with ACS. The mean age was 68.7 ± 8.6 years, with 35.3 % females. 31 patients had major bleeding. Twenty-three of these patients were BARC 3 A, five were BARC 3 B, and three were BARC 3 C. Bleeding history [OR (95 % CI), 2.46 (1.02-5.94), p = 0.021], hemoglobin levels [OR (95 % CI), 0.54 (0.45-0.63), p < 0.001], and age > 74 years [OR (95 % CI), 1.03 (1.01-1.06), p = 0.039] were independent predictors of major bleeding. The ORBIT score was an independent predictor of major bleeding in the multivariate analysis: continuous variables [OR (95 % CI), 2.53 (2.61-3.95), p < 0.001] and risk categories [OR (95 % CI), 3.06 (1.69-5.52), p < 0.001]. Comparison of c-indexes for major bleeding events revealed a non-significant difference for the discriminative ability of the two tested scores (p = 0.07) with a continuous NRI of 6.6 % (p = 0.026) and an IDI of 4.2 % (p < 0.001). Conclusion: In ACS patients, the ORBIT score independently predicted major bleeding.Presentation Diyastolik Disfonksiyon Tanısında Elektrokardiyografik Diyastolik Endeksinin Prognostik Rolü(2023) Günlü, SerhatAmaç: Sol ventrikülün diyastolik disfonksiyonu (LVDD), korunmuş ejeksiyon kalp yetmezliği olan bireylerde baskın etiyolojidir. Yüksek tansiyon miyokardda yapısal anormalliklere neden olur ve LVDD'nin seyrini hızlandırır. EKG özelliklerinden belirlenen elektrokardiyografik diyastolik indeks (EDI), sol ventrikül hipertrofisi ile LVDD'nin varlığı arasındaki bağlantı hakkında bilgi verebilir. Bu çalışmanın amacı, hipertansif bireylerde LVDD'yi tanımlamak için EDI göstergesini belirlemekti. Metod: Bu araştırmaya 2022 yılının Ocak ve Aralık ayları arasında sırayla 162 hipertansif hasta dahil edildi. Hastalar, LVDD'si olan ve olmayanlar olarak ayrıldı. [aVL R genliği (V1S genliği + V5R genliği)/PWLI genliği], EDI için formüllerdir. ROC eğrisi analizi kullanılarak, EDI'nin LVDD için öngörü değeri değerlendirildi. Tek değişkenli ve çok değişkenli lojistik regresyon analizi kullanılarak, LVDD'nin bağımsız faktörleri değerlendirildi. İki çok değişkenli model kullanıldı (model I: sürekli değişken olarak EDI ve kategorik değişken olarak model II). Sonuç: Hastalar LVDD olup olmamasına göre iki gruba ayrıldı (LVDD'si olmayan 85 hasta, grup 1; LVDD'si olan 77 hasta, grup 2). Araştırma örnekleminin ortalama yaşı 49±14 idi ve hastaların %42,6'sı erkekti. Çalışmaya katılanların EDI düzeyi 8,50±7,30 idi (Tablo 1). Tablo 1. Clinicalcharacteristics of the studypopulation PARAMETERS LVDD (-) n=85 LVDD (+) n=77 P-value Age (Years) 52.7±1.4 46.1±2.3 0.018 Gender, male, n(%) 28 (33.2) 40 (52.6) 0.009 Smoking, n (%) 36 (41.9) 39 (50.5) 0.305 Diabetesmellitus, n (%) 9 (10.5) 17 (22.7) 0.033 LVEDD, mm 46±4 46±3 0.124 LVESD, mm 28±3 29±2 0.057 IVST, mm 1.0±0.1 1.1±0.2 <0.001 LVEF, % 62±5 60±3.5 0.028 LA, mm 35±4 36±3 0.031 E/A ratio 1.4±0.3 0.9±0.5 <0.001 D1 P waveamplitude, mV 0.1±0.04 0.1±0.05 0.181 aVL R amplitude, mV 0.3±0.3 0.5±0.3 <0.001 V1S amplitude, mV 0.7±0.4 0.7±0.5 0.043 V5R amplitude, mV 1.0±0.5 1.1±0.7 0.093 V1S +V5R amplitude, mV 1.7±0.7 2.0±0.9 0.005 EDI 5.2±3.7 10.6±8.5 <0.001 LVEDD: Leftventricularend-diastolicdimension, LVESD: Leftventricularend-systolicdimension, IVST: Interventricularseptumthickness, LVEF: Leftventricularejectionfraction, LA: Leftatrial, EDI: ElectrocardiographicDiastolic Index. Grup 2'nin EDI puanı, grup 1'inkinden önemli ölçüde daha yüksekti (p <0.001). LVDD'yi tahmin etmek için EDI eğrisi altında kalan alan %0,752 olarak hesaplandı (%95 güven aralığı = 0,651-0,853; p<0,001) (Şekil 1). Şekil 1. ROC analysis of the EDI toestimatediastolicdysfunction EDI eşik değeri 7,4 mV'den büyük olduğunda, LVDD'yi %70'lik bir duyarlılık ve %69'luk bir özgüllükle tahmin eder. Tek değişkenli lojistik regresyon kullanılarak LVDD, EDI ile ilişkilendirildi [OR=1,248, %95 güven aralığı (CI)=1,159 - 1,345, p <0,001]. EDI'yi hem sürekli değişken hem de kategorik değişken olarak incelemek için iki farklı çok değişkenli regresyon modeli oluşturuldu. Her iki modelde de EDI'nin LVDD'nin erken bir göstergesi olduğu ortaya çıktı. Tartışma: Sol atriyal boyutlardaki değişikliklere tipik olarak septal veya arka sol ventrikül duvar kalınlığında bir artış eşlik eder ve bu da sonunda sol ventrikülün hipertrofisi veya yeniden şekillenmesi olarak kendini gösterir. Bu sonuçlar oldukça yaygın olduğundan ve hipertansif kalp hastalığı olan bireylerde artış gösterdiğinden, DD'li hastalarda görülen en yaygın anormalliklerden biridir. Birden fazla grup, DD'de sol ventrikül hipertrofisini ve anlamlı kardiyomiyosit hipertrofisinin histolojik kanıtları ve normalden daha büyük bir sol ventrikül kas kütlesi ile sistolik fonksiyonun korunduğu kalp yetmezliğini belgelemiştir. Arteriyel hipertansiyonu olan bireylerde, uzamış QRS ve QT/QTc aralığı gibi elektrokardiyografik karakteristiklerin genişlemiş bir sol ventrikül kas kütlesini düşündürdüğü bilinmektedir. Bu, DD ve QTc süresinin Doppler'den türetilen parametreleri arasında bir korelasyon olduğunu gösteren önceki çalışmalarla uyumludur. İkincisi ayrıca, uzun QT aralığı ile anormal mekanik fonksiyon arasındaki ilişkinin gözlemlendiği ve hayvan ve hücresel deneylerle desteklendiği kalıtsal uzun QT Sendromları kapsamındaki hastalar için literatürde kapsamlı bir şekilde tartışılmıştır. Patofizyolojik olarak, aksiyon potansiyeli süresinin uzaması, hücre içi kalsiyum birikimi yoluyla belirgin mekanik işlev bozukluğuna neden olabilir. Bununla birlikte, yukarıda belirtilen analizlerin tanısal performansının yanı sıra korelasyonu da, muhtemelen yalnızca bir elektrokardiyografik parametre kullanılarak belirli bir derecede basitleştirme nedeniyle oldukça mütevazıydı. Aslında, aynı grup tarafından daha yeni bir analizde önerildiği gibi, QTc uzamasına Ttepe – Eğilim aralığının uzaması neden olabilir. Önceki çalışmalardan farklılık büyük olasılıkla, ilkinde psödonormal ve/veya kısıtlayıcı dolum paterni olan hastaların daha büyük yüzdesi ile açıklanabilir, bu da daha ileri bir kardiyak hastalık aşamasını ve dolayısıyla daha belirgin repolarizasyon değişikliklerini düşündürür. Tedavi: EDI, ucuz olması, kolayca bulunabilmesi ve uygulanmasının basit olması nedeniyle hipertansiyon nedeniyle takip edilen bireylerde DD'yi tahmin etmek için önemli bir tarama modelidir.Article Citation - WoS: 2Citation - Scopus: 3The effect of body mass index on complications in cardiac implantable electronic device surgery(WILEY, 2023) Güzel, Tuncay; Demir, Muhammed; Aktan, Adem; Kılıç, Raif; Arslan, Bayram; Günlü, Serhat; Altıntaş, Bernas; Karahan, Mehmet Zülkif; Özbek, Mehmet; Aslan, Burhan; Arpa, Abdulkadir; Coşkun, Mehmet Sait; Altunbaş, Mahsum; Tüzün, Rohat; Akgümüş, Alkame; Karadeniz, Muhammed; Aydın, Saadet; Güzel, Hamdullah; Aslan, Selen Filiz; Söner, Serdar; Taş, Ahmet; Ertaş, FarukBackground: Cardiac implantable electronic device (CIED) procedures are prone to complications. In our study, we investigated the effect of body mass index (BMI) on CIED-related complications. Methods: 1676 patients who had undergone CIED surgery (de novo implantation, system upgrade, generator change, pocket revision or lead replacement) at two heart centers in Turkey and met the study criteria were included in our study. For analysis of primary and secondary endpoints, patients were classified as non-obese (BMI < 25 kg/m2), overweight (25 ≤ BMI < 30 kg/m2), and obese (BMI ≥ 30 kg/m2). The primary endpoint was accepted as cumulative events, including the composite ofclinically significant hematoma (CSH), pericardial effusion or tamponade, pneumoth- orax, and infection related to the device system. Secondary outcomes included each component of cumulative events. Results: The rate of cumulative events, defined as primary outcome, was higher in the obese patient group, and we found a significant difference between the groups (3.0%, 4.3%, 8.9%, p = .001). CSH and pneumothorax rates were significantly higher in the obese patient group (0.3%, 0.9%, 1.9%, p = .04; 1.0%, 1.4%, 3.3%, p = .04, respectively). According to our multivariate model analysis; gender (OR:1.882, 95%CI:1.156–3.064, p = .01), hypertension (OR:4.768, 95%CI:2.470–9.204, p < .001), BMI (OR:1.069, 95%CI:1.012–1.129, p = .01) were independent predictors of cumulative events rates. Conclusions: Periprocedural complications associated with CIED (especially hematoma and pneumothorax) are more common in the group with high BMI.Article Citation - Scopus: 7The effect of coronary slow flow on ventricular repolarization parameters(ScienceDirect, 2023) Karahan, Mehmet Zülkif; Aktan, Adem; Güzel, Tuncay; Günlü, Serhat; Kılıç, RaifIntroduction: Ischemia due to microvascular dysfunction may be responsible for the heterogeneity of ventricular repolarization in coronary slow flow. To our knowledge, there is no study in which QT interval, Tp-Te interval, index of cardiac-electrophysiological balance (iCEB), and frontal QRS-T angle were evaluated together in patients with CSF. In this study, we examined for the first time the relationship between all these myocardial repolarization parameters and CSF. Materials and methods: The study group included 178 patients (99 female, mean age: 50.6 ± 8.6 years) with isolated CSF without stenotic lesions and with angiographically proven normal coronary arteries. The control group included 120 patients (71 female, mean age: 49.3 ± 9.4 years) with normal coronary angiography. QRS duration, QT interval, QTc interval, Tp-Te interval, Tp-Te/QT, Tp- Te/QTc, iCEB score, and frontal QRS-T angle were calculated from 12‑lead ECGs. Results: There was no significant difference in demographic parameters between the two groups. Compared with the control group, patients with CSF had significantly longer QTmax duration, QT dispersion, Tp-Te interval, and higher iCEB score, wider frontal QRS-T angle. Conclusion: In our study, we found that many of the ventricular repolarization parameters were adversely affected in patients with CSF. Impaired parameters may be associated with the risk of malignant ventricular arrhythmias.
- «
- 1 (current)
- 2
- 3
- »

