Karahan, Mehmet Zülkif
Loading...

Profile URL
Name Variants
Job Title
Prof. Dr.
Email Address
Main Affiliation
Department of Internal Medical Sciences / Dahili Tıp Bilimleri Bölümü
Status
Current Staff
Website
ORCID ID
Scopus Author ID
Turkish CoHE Profile ID
Google Scholar ID
WoS Researcher ID
Sustainable Development Goals
17
PARTNERSHIPS FOR THE GOALS

0
Research Products
2
ZERO HUNGER

0
Research Products
5
GENDER EQUALITY

0
Research Products
6
CLEAN WATER AND SANITATION

0
Research Products
13
CLIMATE ACTION

0
Research Products
10
REDUCED INEQUALITIES

1
Research Products
16
PEACE, JUSTICE AND STRONG INSTITUTIONS

0
Research Products
8
DECENT WORK AND ECONOMIC GROWTH

0
Research Products
15
LIFE ON LAND

0
Research Products
3
GOOD HEALTH AND WELL-BEING

9
Research Products
9
INDUSTRY, INNOVATION AND INFRASTRUCTURE

0
Research Products
14
LIFE BELOW WATER

1
Research Products
4
QUALITY EDUCATION

0
Research Products
1
NO POVERTY

0
Research Products
7
AFFORDABLE AND CLEAN ENERGY

0
Research Products
11
SUSTAINABLE CITIES AND COMMUNITIES

0
Research Products
12
RESPONSIBLE CONSUMPTION AND PRODUCTION

0
Research Products

This researcher does not have a Scopus ID.

This researcher does not have a WoS ID.

Scholarly Output
26
Articles
24
Views / Downloads
130/3787
Supervised MSc Theses
0
Supervised PhD Theses
0
WoS Citation Count
16
Scopus Citation Count
19
WoS h-index
2
Scopus h-index
3
Patents
0
Projects
0
WoS Citations per Publication
0.62
Scopus Citations per Publication
0.73
Open Access Source
19
Supervised Theses
0
Google Analytics Visitor Traffic
| Journal | Count |
|---|---|
| Cureus | 4 |
| Artuklu International Journal of Health Sciences | 2 |
| International Journal of Cardiovascular Sciences | 2 |
| Journal of Electrocardiology | 2 |
| Dicle Tıp Dergisi | 2 |
Current Page: 1 / 4
Scopus Quartile Distribution
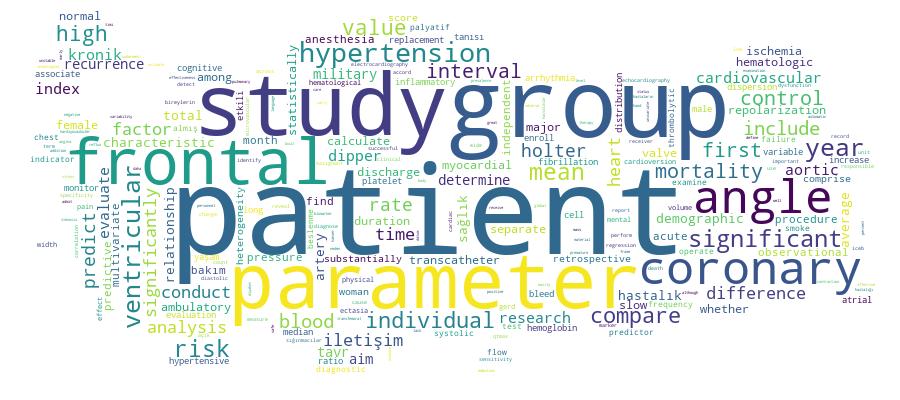
Competency Cloud
26 results
Scholarly Output Search Results
Now showing 1 - 10 of 26
Book Part Kardiyovasküler Hastalıklarda Beslenme(2023) Kayan, Fethullah; Karahan, Mehmet ZülkifBölüm 20 - Kardiyovasküler Hastalıklarda Beslenme ............................................................ 399 Fethullah Kayan - M. Zülkif Karahan 1. Genel Bakış ........................................................................................................................ 400 2. Besinler .............................................................................................................................. 403 3. Gıdalar ............................................................................................................................... 405 xv 4. Hipertansiyon ve Beslenme................................................................................................ 408 5. Obezite-Diyabetüs Mellitüs ve Beslenme ........................................................................... 409 6. Kalp Yetmezliği ve Beslenme.............................................................................................. 410 7. Koroner Arter Hastalığı ve Beslenme .................................................................................. 411 Kaynaklar................................................................................................................................... 413Article Citation - WoS: 2Citation - Scopus: 2Evaluation of Hematological Parameters After Transcatheter Aortic Valve Replacement(Sage Journals, 2023) Karahan, Mehmet Zülkif; Aktan, Adem; Güzel, Tuncay; Kılıç, Raif; Günlü, Serhat; Demir, Muhammed; Ertaş, FarukAlthough transcatheter aortic valve replacement (TAVR) is safe and effective, mortality and bleeding events post procedure are important. The present study investigated the changes in hematologic parameters to evaluate whether they predict mortality or major bleeding. We enrolled 248 consecutive patients (44.8% male; mean age 79.0 ± 6.4 years) undergoing TAVR. In addition to demographic and clinical examination, blood parameters were recorded before TAVR, at discharge, 1 month and 1 year. Hemoglobin levels before TAVR 12.1 ± 1.8 g/dL, 10.8 ± 1.7 g/dL at discharge, 11.7 ± 1.7 g/dL at first month, 11.8 ± 1.4 g/dL at first year (Hemoglobin values compared with pre-TAVR, P < .001, P = .019, P = .047, respectively). Mean platelet volume (MPV) before TAVR 8.72 ± 1.71 fL, 8.16 ± 1.46 fL at discharge, 8.09 ± 1.44 fL at first month, 7.94 ± 1.18 fL at first year (MPV values compared with pre-TAVR, P < .001, P < .001, P < .001, respectively). Other hematologic parameters were also evaluated. Hemoglobin, platelet count, MPV, and red cell distribution width before the procedure, at discharge, and at the first year did not predict mortality and major bleeding in receiver operating characteristic analysis. After multivariate Cox regression analysis, hematologic parameters were not independent predictors of in-hospital mortality, major bleeding, and death at 1 year after TAVR.Article Citation - WoS: 2Non-Dipper Blood Pressure Impact on Coronary Slow Flow in Hypertensive Patients With Normal Coronary Arteries(Cureus, 2023) Özen, Kaya; Karahan, Mehmet ZülkifObjective: Coronary slow flow (CSF) is linked to myocardial ischemia, malignant arrhythmias, and cardiovascular mortality. On the other hand, hypertension (HTN) is an important risk factor for vascular disorders. There is limited research on the relationship between CSF and HTN. This study aimed to investigate TIMI frame count (TFC), which is an indicator of CSF, in dipper and non-dipper hypertensive individuals with normal coronary arteries. Methods: The study was conducted as a retrospective observational study. Patients diagnosed with CSF and dipper or non-dipper hypertension were included in this study. Blood tests were routinely conducted for all patients. ECG was conducted for each patient, and echocardiography was performed. Coronary artery images were obtained in the CAG laboratory. Blood pressure (BP) measurements were obtained from the ambulatory Holter records. The patients were separated into two groups based on ambulatory Holter monitoring. The relationship between CSF and HTN was also examined. Results: A total of 71 patients, comprising 25 women (37.2%) and 46 men (62.8%) with an average age of 52.75±9.42 years, were enrolled in the research. Based on ambulatory BP, the individuals were separated into two groups: non-dipper (n=36) and dipper (n=35). The pulse rate was significantly higher in the non-dipper group (p<0.001). In terms of mean systolic and diastolic blood pressure, there were no substantial differences across the groups (p = 0.326 and p = 0.654, respectively). The daytime mean systolic and diastolic BP did not significantly differ across the groups (p = 0.842 and p = 0.421). The dipper group had substantially lower nighttime systolic and diastolic BP values (p <0.001). The LAD, Cx, and RCA TIMI frame scores were significantly lower in the dipper group (p<0.001). Conclusion: In this study, non-dipper patients had a greater CSF rate than dipper.Article Citation - WoS: 3The prognostic value of ORBIT risk score in predicting major bleeding in patients with acute coronary syndrome(ELSEVIER, 2023) Günlü, Serhat; Arpa, Abdulkadir; Kayan, Fethullah; Güzel, Tuncay; Kılıç, Raif; Aktan, Adem; Bernas, Altıntaş; Karahan, Mehmet ZülkifBackground: The most significant adverse effect of antithrombotic medication in acute coronary syndrome (ACS) is major bleeding, which is related to increased mortality. Studies on ORBIT risk score in predicting major bleeding in ACS patients are limited. Objective: This research aimed to examine whether the ORBIT score calculated at the bedside can identify major bleeding risk in patients with ACS. Methods: This research was retrospective, observational, and conducted at a single center. Analyses of receiver operating characteristics (ROC) were utilized to define the diagnostic value of CRUSADE and ORBIT scores. The predictive performances of the two scores were compared using DeLong's method. Discrimination and reclassification performances were evaluated by the integrated discrimination improvement (IDI), and net reclassification improvement (NRI). Results: The study included 771 patients with ACS. The mean age was 68.7 ± 8.6 years, with 35.3 % females. 31 patients had major bleeding. Twenty-three of these patients were BARC 3 A, five were BARC 3 B, and three were BARC 3 C. Bleeding history [OR (95 % CI), 2.46 (1.02–5.94), p = 0.021], hemoglobin levels [OR (95 % CI), 0.54 (0.45–0.63), p < 0.001], and age > 74 years [OR (95 % CI), 1.03 (1.01–1.06), p = 0.039] were independent predictors of major bleeding. The ORBIT score was an independent predictor of major bleeding in the multivariate analysis: continuous variables [OR (95 % CI), 2.53 (2.61–3.95), p < 0.001] and risk categories [OR (95 % CI), 3.06 (1.69–5.52), p < 0.001]. Comparison of c-indexes for major bleeding events revealed a non-significant difference for the discriminative ability of the two tested scores (p = 0.07) with a continuous NRI of 6.6 % (p = 0.026) and an IDI of 4.2 % (p < 0.001). Conclusion: In ACS patients, the ORBIT score independently predicted major bleeding.Article Citation - Scopus: 1The predictive effect of shock index on mortality in patients with acute heart failure(AME Publishing, 2023) Günlü, Serhat; Kayan, Fethullah; Karahan, Mehmet ZülkifBackground: The predictive usefulness of the shock index (SI), which is determined as a proportion of heart rate (HR) to systolic blood pressure (SBP), and age-adjusted SI (SI × age) for clinical outcomes other than mortality in acute heart failure (AHF) is not well established. This research aimed to examine whether SI and SI × age measured non-invasively at a patient’s bedside can identify mortality risk in patients admitted to the coronary care unit (CCU) with AHF. Methods: This research was carried out as a retrospective case-control study. Indices were calculated. The receiving operating characteristic (ROC) and Youden index were applied to calculate the optimal SI and SI × age cut-off for estimating mortality. Using multivariate analysis to determine independent indicators of mortality in patients with AHF. Results: A total of 1,468 patients who were hospitalized at the CCU with AHF were included. The population’s median age was 81 (73–91) years and 53.7% were male. In the survivor group, the median SI was 0.6 (0.5–0.75), and the median SI × age was 46 (38–58). In the non-survivor group, the median SI was 0.62 (0.55–0.81) and the median SI × age was 53 (44–66). According to the Youden index, the best value of SI was 0.56 with a specificity of 46% and a sensitivity of 70%, and the best value of SI × age was 44.8 with a specificity of 48% and a sensitivity of 76%. In the multivariate analysis, the power of SI × age to predict mortality was 2.39 times greater than other independent predictors. Conclusions: SI and SI × age calculated in the CCU may be valuable prognostic markers for identifying AHF patients at high risk for adverse outcomes.Book Part KRONİK HASTALIĞI OLAN BİREY VE AİLE İLE İLETİŞİM(2023) Aktan, Adem; Karahan, Mehmet ZülkifKronik hastalık, uzun süreli tedavi gerektiren ve hayatı boyunca sürebilecek bir sağlık durumunu ifade eder. Bunlar, diyabet, hipertansiyon, kalp hastalığı, kanser, multipl skleroz gibi bir dizi farklı hastalığı içerebilir. Kronik hastalık tanısı alan bireylerin ve ailelerin yaşamlarında büyük bir etkiye sahip olabilir ve duygusal, sosyal ve fiziksel zorluklara neden olabilir. Bu nedenle, kronik hastalık tanısı almış bireylerle ve aileleriyle iletişim kurarken dikkatli ve duyarlı olmak önemlidir (1). İletişim, bireylerin duygularını ifade etmelerine, endişelerini paylaşmalarına ve birbirleriyle destek sağlamalarına yardımcı olabilir. Kronik hastalıkla ilgili iletişim becerileri, bireylerin sağlıklı bir şekilde başa çıkmalarına ve daha iyi sonuçlar elde etmelerine yardımcı olabilir. Kronik hastalık tanısı almış bireyler ve aileleri arasındaki iletişim, aşağıdaki bazı temel prensiplere dikkat ederek etkili bir şekilde gerçekleştirilebilir: Açık iletişim kurma: Kronik hastalık tanısı almış bir bireyin ve ailesinin duygularını ve deneyimlerini anlamak için empati kurmak önemlidir. Açık iletişim, dürüst, saygılı ve etkili bir iletişim tarzını içerir. Kronik hastalık tanısı almış bir birey ve ailesiyle iletişim kurarken açık ve net olmak önemlidir. VII. Sonuç Kronik hastalık tanısı almış bireyler ve aileleriyle etkili iletişim kurmak önemlidir. Etkili iletişim, hastaların sağlık sonuçlarını, yaşam kalitesini ve memnuniyetini artırabilir. Ailelerin de katılımıyla birlikte, uygun tıbbi bakım sağlanabilir ve sağlıklı bir iyileşme süreci desteklenebilir. Bu nedenle, sağlık profesyonellerive diğer ilgili paydaşlar, hastalarla etkili iletişim kurma becerilerini geliştirmek için yönlendirilmelidir. Kronik hastalık yönetiminde etkili iletişim, hastaların ve ailelerinin gereksinimlerini anlamak ve onları desteklemek için vazgeçilmez bir araçtır.Article Citation - WoS: 2The Significance of Frontal Plane QRS-T Angle for Estimating Non-Dipper Hypertension(Cureus, 2022) Evsen, Ali; Karahan, Mehmet ZülkifObjective: The frontal QRS-T angle (fQRS-T) is linked to myocardial ischemia and ventricular arrhythmias. On the other hand, non-dipper hypertension is a risk factor for cardiac adverse events. The objective of this research was to determine whether the fQRS-T, a marker of ventricular heterogeneity, could be used to predict non-dipper hypertensive individuals in the lack of left ventricular hypertrophy. Methods: The observational study was carried out retrospectively. Patients diagnosed with hypertension were included in this study. Blood tests were routinely conducted for all patients. Electrocardiography (ECG) was conducted for each patient and echocardiography was performed. Blood pressure (BP) values were collected from the ambulatory Holter records. According to ambulatory Holter monitoring, the individuals were separated into two groups. The association between fQRS-T and hypertension was investigated. Results: The research involved 123 patients, with an average age of 51.85±8.22 years, comprising 76 women (61.8%) and 47 males (38.2%). According to ambulatory Holter monitoring, patients were separated into dippers (n=65) and non-dippers (n=58). There were no statistically significant in the laboratory and echocardiographic variables (p>0.05). QT dispersion (QTd) and fQRS-T were substantially greater in the non-dipper group than in the dipper group (p=0.043 and p<0.001, respectively). Independent determinants of non-dipper status were determined by univariate and multivariate logistic regression analyses. fQRS-T was found to be the only independent indicator of non-dipper status (OR: 1.03, 95%CI: 1.02-1.06, p<0.001). Conclusion: The fQRS-T may be a useful marker for estimating non-dipper hypertensive individuals in the lack of left ventricular hypertrophy.Article Citation - WoS: 3Citation - Scopus: 3The prognostic value of ORBIT risk score in predicting major bleeding in patients with acute coronary syndrome(ScienceDirect, 2023) Günlü, Serhat; Arpa, Abdulkadir; Kayan, Fethullah; Güzel, Tuncay; Kılıç, Raif; Aktan, Adem; Altintaş, Bernas; Karahan, Mehmet ZülkifBackground: The most significant adverse effect of antithrombotic medication in acute coronary syndrome (ACS) is major bleeding, which is related to increased mortality. Studies on ORBIT risk score in predicting major bleeding in ACS patients are limited. Objective: This research aimed to examine whether the ORBIT score calculated at the bedside can identify major bleeding risk in patients with ACS. Methods: This research was retrospective, observational, and conducted at a single center. Analyses of receiver operating characteristics (ROC) were utilized to define the diagnostic value of CRUSADE and ORBIT scores. The predictive performances of the two scores were compared using DeLong's method. Discrimination and reclassification performances were evaluated by the integrated discrimination improvement (IDI), and net reclassification improvement (NRI). Results: The study included 771 patients with ACS. The mean age was 68.7 ± 8.6 years, with 35.3 % females. 31 patients had major bleeding. Twenty-three of these patients were BARC 3 A, five were BARC 3 B, and three were BARC 3 C. Bleeding history [OR (95 % CI), 2.46 (1.02-5.94), p = 0.021], hemoglobin levels [OR (95 % CI), 0.54 (0.45-0.63), p < 0.001], and age > 74 years [OR (95 % CI), 1.03 (1.01-1.06), p = 0.039] were independent predictors of major bleeding. The ORBIT score was an independent predictor of major bleeding in the multivariate analysis: continuous variables [OR (95 % CI), 2.53 (2.61-3.95), p < 0.001] and risk categories [OR (95 % CI), 3.06 (1.69-5.52), p < 0.001]. Comparison of c-indexes for major bleeding events revealed a non-significant difference for the discriminative ability of the two tested scores (p = 0.07) with a continuous NRI of 6.6 % (p = 0.026) and an IDI of 4.2 % (p < 0.001). Conclusion: In ACS patients, the ORBIT score independently predicted major bleeding.Article Serum Ürik Asit, Kronik Total Oklüzyon'a PCI Yapıldığında, Kontrast Maddeye Bağlı Nefropatiyi Öngörür(2025) Kayan, Fethullah; Karahan, Mehmet ZülkifAmaç : CIN (kontrast kaynaklı nefropati), CTO (kronik total oklüzyon) için yapılan PCI (perkütan koroner girişim) sonrasında görülen önemli bir komplikasyondur. Yükselmiş serum ürik asit (SUA) düzeylerinin böbrek hasarında rol oynadığı bildirilmiştir, ancak CTO-PCI hastalarında CIN için öngörücü değerleri net değildir. Bu çalışma, SUA düzeyleri ile CIN riski arasındaki ilişkiyi bu hasta grubunda incelemeyi amaçlamıştır. Yöntemler: Bu retrospektif gözlemsel çalışmaya, Nisan 2017 – Mart 2023 tarihleri arasında Diyarbakır Gazi Yaşargil Eğitim ve Araştırma Hastanesi’nde CTO nedeniyle PCI uygulanan 225 hasta dahil edilmiştir. Hastalar, başlangıçtaki SUA düzeylerine göre üç gruba ayrılmıştır: ≤5.2 mg/dL (n=75), 5.3–6.6 mg/dL (n=75) ve ≥6.7 mg/dL (n=75). CIN, PCI sonrası 48–72 saat içinde serum kreatinin düzeyinde %25’ten fazla artış olarak tanımlanmıştır. Klinik, demografik ve laboratuvar parametreleri ki-kare, ANOVA veya Kruskal-Wallis testleriyle karşılaştırılmıştır. SUA’nın CIN için öngörücü değerini belirlemek amacıyla lojistik regresyon ve ROC analizleri uygulanmıştır. Bulgular: CIN, 44 hastada (%19,6) gelişmiştir. Yüksek SUA düzeyleri; artmış CIN insidansı (p<0.001), daha yüksek kronik böbrek hastalığı prevalansı (p<0.001), düşük ejeksiyon fraksiyonu (EF) (p=0.027) ve artmış mortalite (p=0.023) ile ilişkili bulunmuştur. ROC analizi, 5.95 mg/dL SUA kesim değerini belirlemiştir (AUC=0.643, %95 GA: 0.561–0.725, p=0.003) — bu değer için duyarlılık %72.7 ve özgüllük %56.4 olarak saptanmıştır. Tek değişkenli analizde yaş, EF, C- reaktif protein ve SUA CIN’in anlamlı belirteçleri olarak saptanmış, ancak çok değişkenli analizde anlamlılıklarını korumamışlardır. Sonuç: Yüksek SUA düzeyleri, CTO-PCI hastalarında artmış CIN riski ile ilişkilidir. Rutin SUA değerlendirmesi, yüksek riskli hastaların erken tanımlanmasına yardımcı olabilir ve önleyici stratejilerin güçlendirilmesini destekleyebilir.Article Citation - WoS: 2Citation - Scopus: 3The effect of body mass index on complications in cardiac implantable electronic device surgery(WILEY, 2023) Güzel, Tuncay; Demir, Muhammed; Aktan, Adem; Kılıç, Raif; Arslan, Bayram; Günlü, Serhat; Altıntaş, Bernas; Karahan, Mehmet Zülkif; Özbek, Mehmet; Aslan, Burhan; Arpa, Abdulkadir; Coşkun, Mehmet Sait; Altunbaş, Mahsum; Tüzün, Rohat; Akgümüş, Alkame; Karadeniz, Muhammed; Aydın, Saadet; Güzel, Hamdullah; Aslan, Selen Filiz; Söner, Serdar; Taş, Ahmet; Ertaş, FarukBackground: Cardiac implantable electronic device (CIED) procedures are prone to complications. In our study, we investigated the effect of body mass index (BMI) on CIED-related complications. Methods: 1676 patients who had undergone CIED surgery (de novo implantation, system upgrade, generator change, pocket revision or lead replacement) at two heart centers in Turkey and met the study criteria were included in our study. For analysis of primary and secondary endpoints, patients were classified as non-obese (BMI < 25 kg/m2), overweight (25 ≤ BMI < 30 kg/m2), and obese (BMI ≥ 30 kg/m2). The primary endpoint was accepted as cumulative events, including the composite ofclinically significant hematoma (CSH), pericardial effusion or tamponade, pneumoth- orax, and infection related to the device system. Secondary outcomes included each component of cumulative events. Results: The rate of cumulative events, defined as primary outcome, was higher in the obese patient group, and we found a significant difference between the groups (3.0%, 4.3%, 8.9%, p = .001). CSH and pneumothorax rates were significantly higher in the obese patient group (0.3%, 0.9%, 1.9%, p = .04; 1.0%, 1.4%, 3.3%, p = .04, respectively). According to our multivariate model analysis; gender (OR:1.882, 95%CI:1.156–3.064, p = .01), hypertension (OR:4.768, 95%CI:2.470–9.204, p < .001), BMI (OR:1.069, 95%CI:1.012–1.129, p = .01) were independent predictors of cumulative events rates. Conclusions: Periprocedural complications associated with CIED (especially hematoma and pneumothorax) are more common in the group with high BMI.
- «
- 1 (current)
- 2
- 3
- »

